Germany's Digital Health Act sparks debate over modernisation and funding gaps
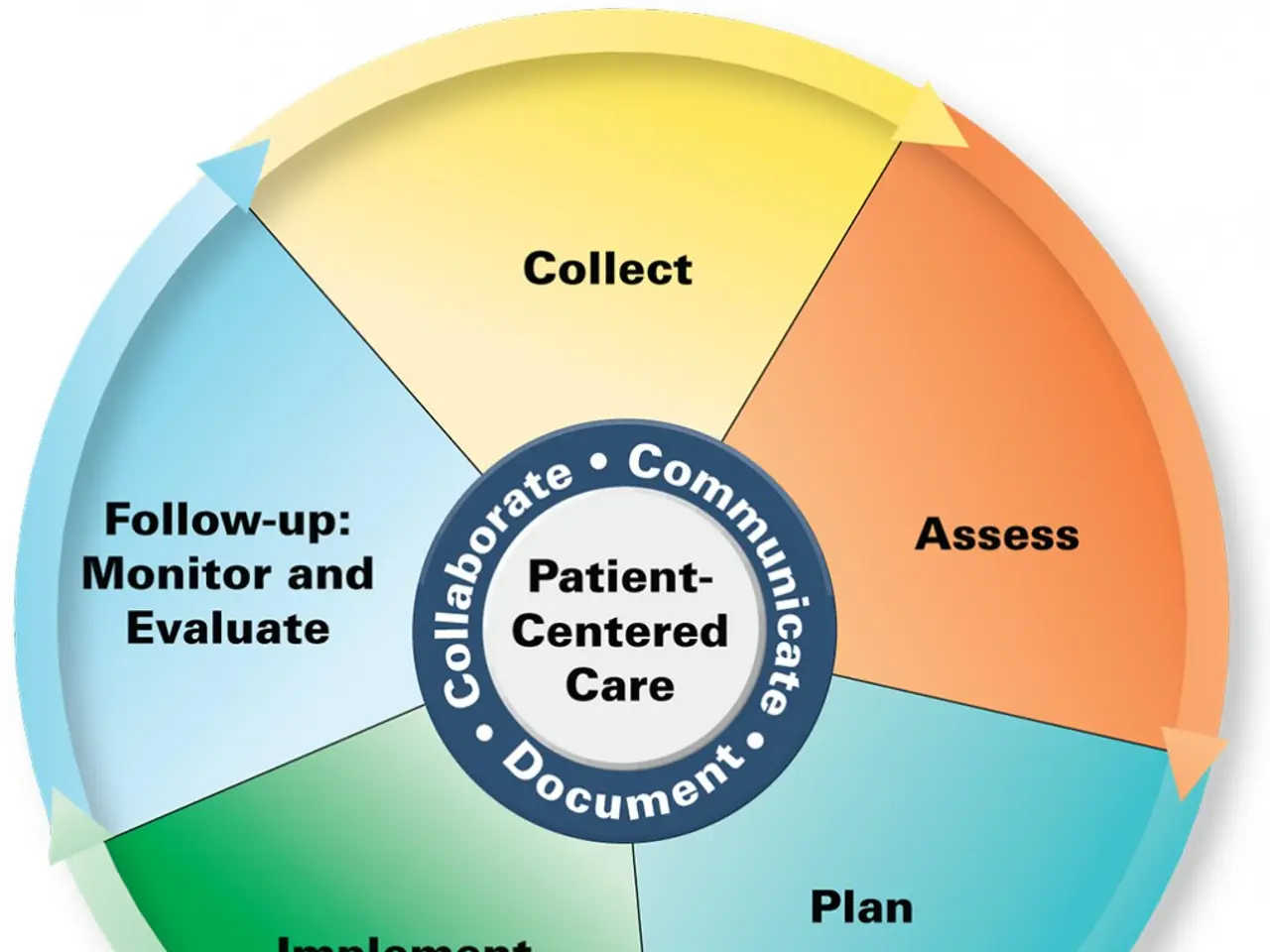
Federal Health Minister Nina Warken (CDU) has presented plans for a new Digital Health Act. The proposals aim to modernise healthcare through better digital tools and infrastructure. Key changes include upgrades to the electronic patient record (ePA) and improvements to the telematics infrastructure (TI).
The announcement has drawn mixed reactions from healthcare providers, insurers, and physicians. While some welcome the reforms, others highlight gaps—particularly in long-term care and data access for research.
The Digital Health Act focuses on four main areas: strengthening the gematik agency, enhancing the ePA, simplifying the TI, and making it more resilient to outages. The gematik, established in 2005, already manages the TI, including the ePA pilot due to launch in January 2025 in regions like Franken, Hamburg, and parts of Nordrhein-Westfalen. A nationwide rollout is planned later that year.
The AOK health insurance fund supports the ePA's expanded functions and wants easier authentication for users. It also backs plans for the Health Research Data Center (FDZ) to use health data more effectively. However, the AOK argues for better access to policyholder data to improve care management. Additionally, it proposes giving the statutory health insurance association (GKV) a larger stake in gematik or granting insurers stronger voting rights in shareholder meetings.
Physicians have responded with cautious optimism but stress that further refinements are needed. The National Association of Statutory Health Insurance Physicians (KBV) is pushing for an independent 'electronic care folder' separate from the ePA. Doctors remain sceptical about the current ePA proposals, insisting that quality and functionality must come first.
Long-term care providers feel sidelined by the reforms. Thomas Knieling, federal managing director of the German Association for the Elderly and Disabled (VDAB), argues that long-term care must be treated as a distinct sector. He calls for practical digital solutions and reliable funding to ensure digitalisation delivers real improvements in daily operations.
Financing disputes have also surfaced. Health insurers, which cover 93% of TI costs, demand more decision-making power and transparency. A court ruling previously confirmed that full reimbursement of TI expenses was never legally guaranteed, adding to ongoing tensions over funding and governance.
The Digital Health Act sets out to improve digital healthcare through stronger infrastructure and expanded data use. Insurers, physicians, and care providers have all raised concerns about implementation and funding.
The next steps will depend on how the government addresses these issues—particularly in long-term care and data access. The success of the reforms may hinge on balancing technological upgrades with practical needs across the healthcare system.
Read also:
- American teenagers taking up farming roles previously filled by immigrants, a concept revisited from 1965's labor market shift.
- Weekly affairs in the German Federal Parliament (Bundestag)
- Landslide claims seven lives, injures six individuals while they work to restore a water channel in the northern region of Pakistan
- Escalating conflict in Sudan has prompted the United Nations to announce a critical gender crisis, highlighting the disproportionate impact of the ongoing violence on women and girls.