India’s insurance delays leave patients stranded in medical emergencies
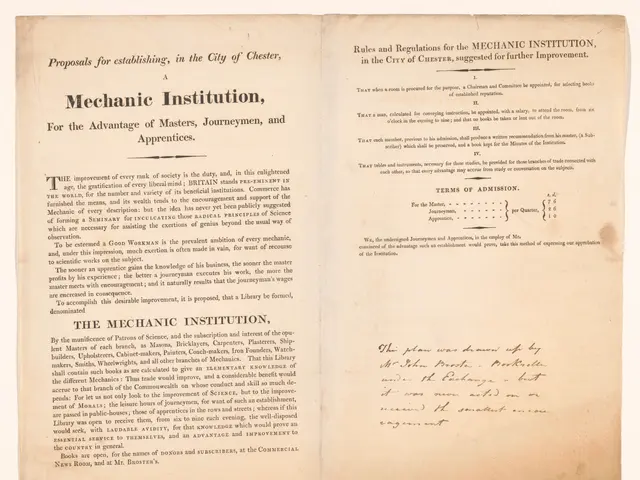
India’s insurance regulator, the Insurance Regulatory and Development Authority of India (IRDAI), is lagging in digital reforms, causing delays and frustration for policyholders. While other countries' regulators use technology to simplify processes, IRDAI still relies on outdated methods. Patients and hospitals continue to face long waits for cashless claims, despite rules meant to expedite settlements.
IRDAI implemented a rule in 2023 mandating insurers to settle cashless claims within three hours. However, compliance remains inconsistent, leaving families in medical emergencies waiting much longer. Hospitals often delay approvals, withhold Explanation of Benefits (EOB) documents, or fail to provide Explanation of Coverage (EOC) statements before admission. These gaps add stress during urgent care situations.
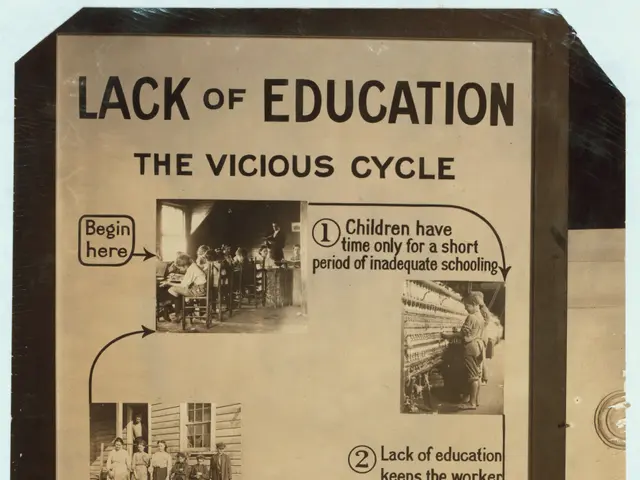
The delays in digital adoption have tangible consequences. Patients face unnecessary stress during emergencies, while insurers grapple with inefficiency and higher costs. Without robust reforms, India’s insurance sector risks falling behind global standards. Faster, more transparent processes could enhance coverage, reduce disputes, and restore public confidence.
Read also:
- American teenagers taking up farming roles previously filled by immigrants, a concept revisited from 1965's labor market shift.
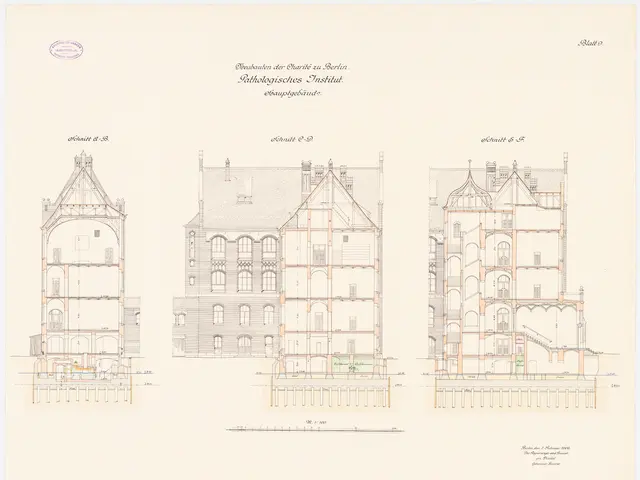
- Weekly affairs in the German Federal Parliament (Bundestag)
- Landslide claims seven lives, injures six individuals while they work to restore a water channel in the northern region of Pakistan
- Escalating conflict in Sudan has prompted the United Nations to announce a critical gender crisis, highlighting the disproportionate impact of the ongoing violence on women and girls.